Applied physiology
A reasonable understanding of pulmonary physiology is elementary in the understanding the approach and bedside management of respiratory disorders. An attempt has been made to synchronize physiological or pathological deviations with ventilatory management.
PHYSIOLOGICAL PRINCIPLES
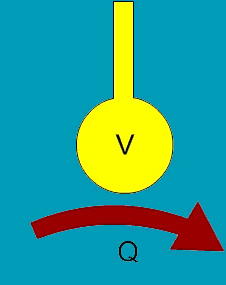
The physiological basis of treating any critical newborn lies in the optimization of ventilation and perfusion.Under ideal conditions, Ventilation and Perfusion are evenly matched and the V/Q ratio = 1. In disease states , complicated by hypoxemia or hypotension , a certain balance has to be struck between ventilation and perfusion
FIGURE 2
V=VENTILATION
Q=PERFUSION
 Blood Pressure
Blood Pressure
O2 content of blood
Dilatation of air sac
Nitric Oxide metabolism
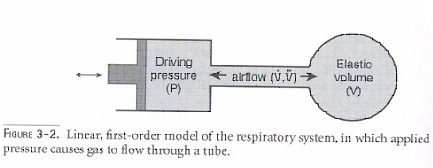
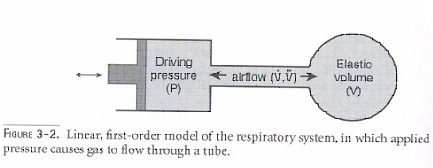
VENTILATION (V):
Ventilation applies to a physiological tidal volume, which reaches the alveoli and distends it optimally. If the minute ventilation ( tidal volume X rate ) is optimal , the ideal CO2 will be 40 to 45 mm of Hg. Normal tidal volume in neonate is 4 to 6 ml / kg .
PERFUSION (Q):
This is maintained by the state of dilatation of the pulmonary arterioles and capillaries supplying the air sac. It is controlled to a large extent by systemic blood pressure (Mean Arterial Blood Pressure). Myocardial pump function determines the systemic blood pressure directly. In addition certain physiological variables have to be taken into consideration.
. Hb content of the blood
. State of dilation of the air sac (FRC)
. Nitric Oxide Metabolism (maintains pulmonary arteriolar dilatation)
Basic Understanding Of Various Lung Units In Disease States
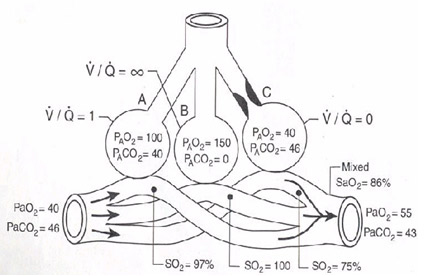
Three-lobe , three -compartment model of the lung with V/Q equal to 1 in A, V/Q equal to infinity in B, and V/Q equal to zero in C . Coming into the pulmonary circuit on the left is blood returning from the body and having a low PaO2 (40mmHg) and a high Pa CO2 (46mm Hg ) . Mixed blood returning from the lungs is not fully saturated with O2 because of venous admixture from the low V/Q unit C , where the lack of ventilation leaves the Pa O2 unchanged (40mmHg ); SO2 of 75% at a PaO2 of 40 mmHg, and a Pa O2 of 55 mmHg at a SaO2 of 86% (Adapted from Goldsmith : Physiological principles pg 56)
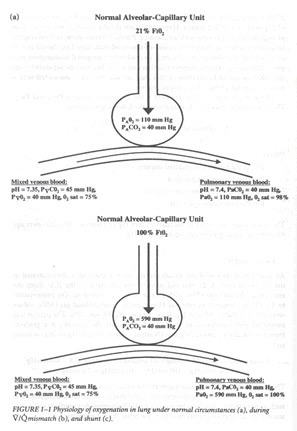
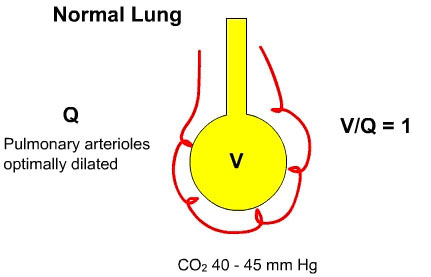
'NORMAL LUNG UNDER IDEAL CONDITIONS'
The pulmonary arterioles unfurl completely and perfuse the alveolar bed completely
V/Q = 1
CO2 40-45 mm Hg
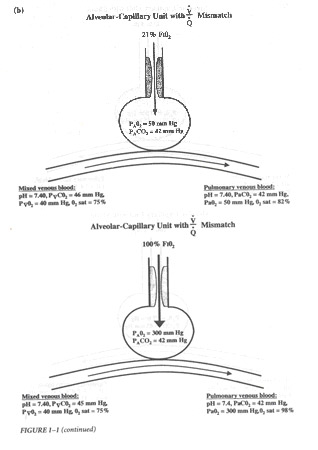
Physiological abnormalities in disease states
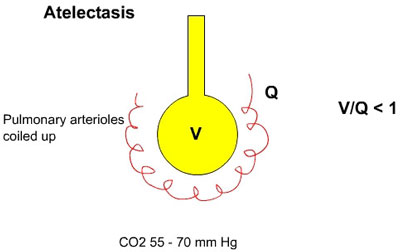
ALVEOLI IS ATELECTATIC
The pulmonary arterioles are coiled up leading to less perfusion to those alveoli (Pulmonary hypertension) and if atelectasis is more profound perfusion proportionately is reduced leading to intrapulmonary shunting due to admixture of mixed venous blood into the systemic circulation. The density of the haziness on the X ray is a rough estimate of the blood CO2 levels .
V/Q< 1
CO2 55-70 mmHg
ALVEOLI ARE OPTIMALLY DISTENDED
ALVEOLAR OVERDISTENTION:
ALVEOLI IS ATELECTATIC
The pulmonary arterioles are coiled up leading to less perfusion to those alveoli (Pulmonary hypertension) and if atelectasis is more profound perfusion proportionately is reduced leading to intrapulmonary shunting due to admixture of mixed venous blood into the systemic circulation. The density of the haziness on the X ray is a rough estimate of the blood CO2 levels .
V/Q< 1
CO2 55-70 mmHg
ALVEOLI ARE OPTIMALLY DISTENDED
ALVEOLAR OVERDISTENTION:
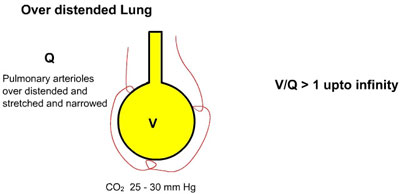
On the other hand if the alveoli is overdistended due to inappropriate pressures on the ventilator (PEEP/CPAP), the pulmonary arterioles got stretched to a point where narrowing of their lumen causing pulmonary hypertension leading, to decreased perfusion in the lung and intrapulmonary shunt. The X Ray shows hyperlucent lung fields . Initial blood gas PaCo2 may be low between 25 and 30 mm of Hg ,but may subsequently get elevated beyond 50 mm of Hg due to inadequate gas exchange and air trapping
V/Q >1 (upto infinity)
CO2 =25-30mmHg
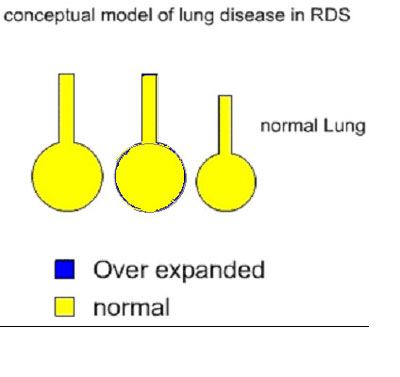
CONCEPTUAL MODELS OF APPLIED PHYSIOLOGY
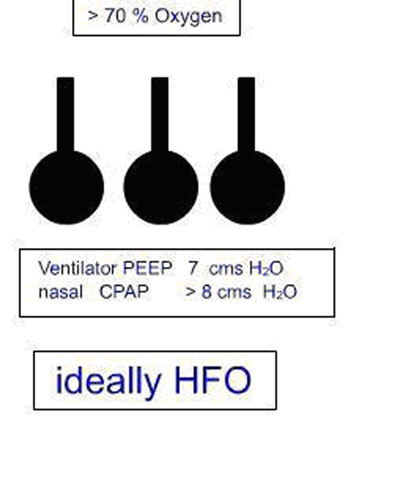
It would be over simplification of the lung units and the surface area for gas exchange by presenting a model of lung units with 3 generations of alveoli, the collapse of which present with increasing oxygen requirements in atelectatic lung disease.
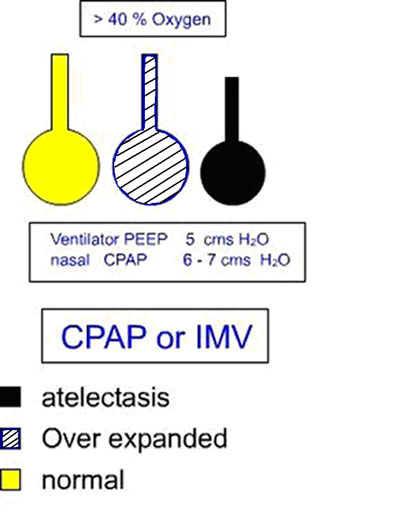
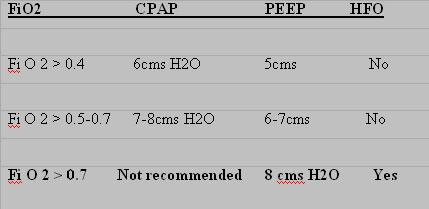
OXYGEN REQUIREMENTS > 40% (FiO2 >0.4)
One generation of alveoli maybe collapsing and it would be appropriate to institute assisted ventilation ideally CPAP or IMV at this stage. This would recruit lung volume and optimize gas exchange and prevent morbidity and air leaks.
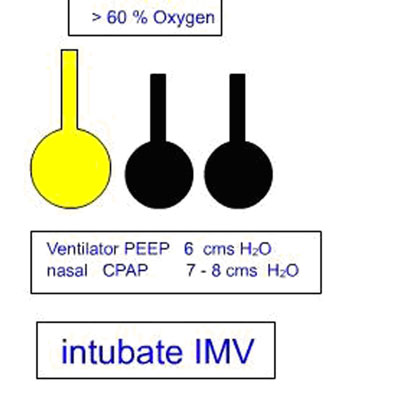
OXYGEN REQUIREMENTS > 60% (FiO2 >0.6)
Two generations of alveoli have collapsed and unless interfered, actively with intubation and ventilation (IMV), air leaks, pulmonary hypertension and morbidity could occur.
OXYGEN REQUIREMENTS > 70-80% (FiO2 >0.7-0.8)
Most generations of alveoli have collapsed and only approximately 1/3 alveolar surface area is available for gas exchange. It would be inadvisable to allow a neonate with RDS to progress to this stage. When ventilation (IMV) is resorted to at this stage air leaks, severe pulmonary hypertension and pulmonary hemorrhage could occur.
From the above discussion it is apparent that EARLY RECRUITMENT OF LUNG VOLUME is essential for optimum ventilation and prevention of lung morbidity. The early and optimal application of PEEP or CPAP in lung disease is the sine qua non of ventilatory care and reflects the great variability in morbidity and mortality of various centers dealing in newborn care. The optimization of FRC by CPAP or PEEP is the most important parameter of neonatal ventilation. A thumb rule in this lung volume recruitment strategy is highlighted below which is basically intended for atelectatic lung disease, which forms the bulk of the spectrum of diseases treated in the NICU.
Back