CPAP
INTRODUCTION
Continuous Positive Pressure is a technique in which a sustained continuous pressure is applied to the airways through out both inspiration and expiration. It recruits lung volume (FRC) prevents atelectasis and opens up collapsed alveoli improving V/Q mismatch and hypoxemia in HMD. In 1971 Gregory and colleagues successfully applied it in HMD in a spontaneously breathing baby. Early use of CPAP may decrease the need for subsequent mechanical ventilation, by optimization of lung volume early in the disease process. 27 28
PHYSIOLOGIC EFFECTS OF CPAP:
Pulmonary effects
1. Increase in functional Residual Capacity (FRC)
2. Increase in alveolar surface area-thereby reducing right to left shunting
3. Alveolar distention will occur with the following effects:
Prevention of atelectasis
Prevention of airway closure and redistribution of fluid within the lung, resulting in an increase in PaO2 and lung compliance,
Reducing of work of breathing (WOB).
CENTRAL EFFECTS:
Influencing the control of breathing by increased central repiratory activity with more regular breathing and a decreased respiratory rate owing to influence via peripheral pulmonary reflexes.
CARDIOVASCULAR EFFECTS: 29 30
low levels of cpap (3-5 cm of H2O)
This does not have a significant effect on heart rate cardiac out put and venous return.
High levels of cpap 8-10cm h20
This causes the following side effects:
Increase in the airway lung resistance
br> Impedence of the systemic venous return and reduction of cardiac out put.
Overdistention of the lung.Increase in the dead space ventilation and dead space/tidal volume ratio(Vd/Vt), resulting in higher Pco2.
Barotrauma,interstitial emphysema ,pneumothorax,pneumomediastinum
CPAP GUIDELINES:
Any Preterm baby less than 33 weeks gestation with repiratory distress and any Preterm less than 30 weeks should receive CPAP 5 cms H2O from the time baby is born and slowly weaned off CPAP if oxygen requirements, respiratory rate and retractions, indicate minimal lung disease.31
CPAP BASIC SYSTEM:
THE CPAP APPARATUS:
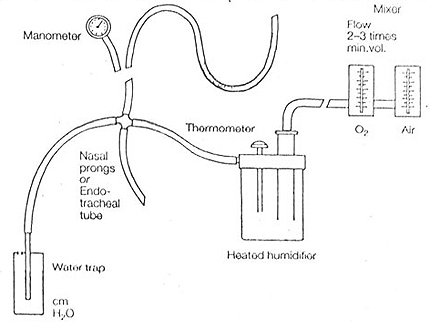
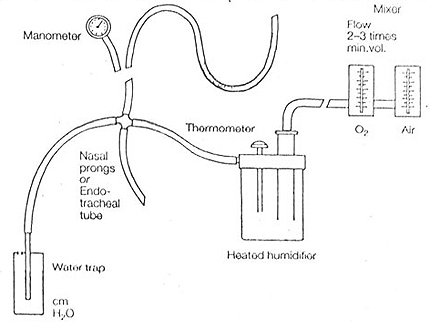
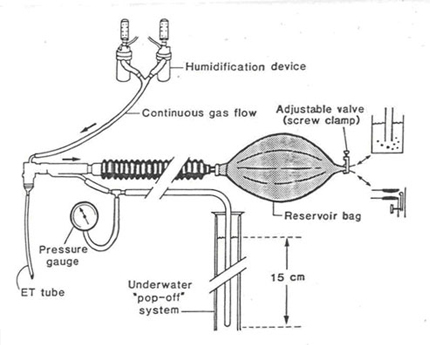
1. Continuous gas flow.
2. A humidification device.
3. A reservoir bag.
4. A valve to produce above ambient expiratory pressure.
5. An underwater pop off system
CPAP DELIVERY SYSTEMS
An ideal CPAP system should have a flow, which is 2 times the minute ventilation of the baby. Fresh gas in the circuit is delivered to the reservoir bag. This would meet the peak inspiratory flow requirements of the baby. The required flow after humidification then passes through a check valve that opens during spontaneous inspiration and closes during expiration. The gas flow to the reservoir bag should be sufficient to keep it fully distended during respiration. Depletion of the bag could lead to increased work of breathing and dead space ventilation. CPAP can be maintained by an underwater tube or a valve. The amount of CPAP can be varied by a change in the amount of obstruction to outflow. The circuit flow should be regulated by observing the movement of the manometer during the infant's inspiration and adjusting it to a level that produces the least pressure deflection towards ambient pressure.
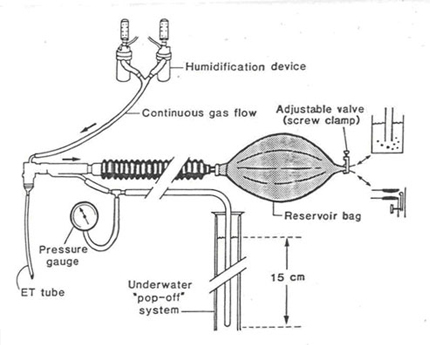
(Adapted from Goldsmith assisted ventilation of the neonate pg 52)
Initiation of CPAP (HMD)
1. Pa O 2 < 50-60 mm Hg in Fi O2 0.4 to 0.7
2. Recurrent apnea
3. Early use of CPAP (5cms H2O) from time of birth is preferred in Preterm babies <30 weeks.
The determination of ideal CPAP
If the infant is not endotracheally intubated, make 1cm H2O increments till grunting and retractions disappear or an audible breath sounds can be heard over the lungs. This is associated with good oxygen saturations above 95-98%.
INDICATIONS OF CPAP:
1) Apnea of prematurity: CPAP 4-5 cms H2O.
1) HMD CPAP 5-7 cms H2O of FiO 2 < O.6.
2) Pneumonia
3) Bronchomalacia.
4) Differentiate lung disease from cardiac disease.
5) Sleep Apnea.
6) Weaning from the ventilator
Caution should be exercised in babies less than 1500 grams IMV should be instituted early in the disease with minimal trial of CPAP if Fi O2 > 0.4 to 0.6 and based on clinical worsening of the distress
GUIDELINES FOR CPAP THERAPY
HMD
• Start with CPAP of 6 cms H2O
• Increments of 2 cms H2 O are done every 15 mins to achieve oxygen saturation above 95% to a maximum of 10 cms H2O by endotracheal tube or 12 cms by noninvasive methods.(Nasopharyngeal CPAP or Nasal prongs)
In our center we opt to go for IMV if the CPAP requirements exceed 7 cms H2O or the FiO2 > 0.6, especially if the baby is less than 1500 gms. In smaller babies it will be better to institute IMV when the FiO2 is more than 0.4
CPAP Failure
• PaO2 < 50% in 100% O2 (FiO2 1.0) with max CPAP
• CPAP levels 10-12 cms H2O
• PH < 7.25
• PCO2 > 50-60 mmHg
Types of CPAP
• Nasal prongs
• Nasopharyngeal (endotracheal tube)
In our center Nasopharyngeal CPAP is used. It is easy to maintain but blockage of tube with secretions is the main problem, leading to increased work of breathing. When nasal prongs are applied constant dislocation is a problem and the baby should have his mouth closed by a chinstrap to prevent loss of CPAP.
Complications of Nasopharyngeal CPAP
1) Pneumothorax
2) Abdominal distension and feed intolerance
3) Nasal irritation and damage to turbinates of nose
Weaning off CPAP:
• Oxygen should be decreased by 3 to 5 % every time the paO2 exceeds 70 mmHg or oxygen saturation exceeds 98 %.
• When FiO2 < 0.4 the CPAP should be reduced by 1 cm H2O every 4-6 hours until a CPAP of 4-5 cms H2O is reached. 32,33
• Transfer to Head box oxygen (keep FiO2 5-10% above what is used on the CPAP initially) Keep saturation > 90-92 in Preterm baby. Adjust oxygen flow rate accordingly.
• Avoid use of 2 mm Endotracheal tube for Nasopharyngeal CPAP (very high work of breathing and extubation failure)
Trouble shooting while on CPAP (Nasopharyngeal)
• Plugged tube: Increasing oxygen requirements, desaturation or apnea. Suction ET tube 4-6 hourly. Change nostril of ET tube daily.
• Malpositioned ET: Bradycardia with movement. Reposition tube in the opposite nasopharynx rather than oropharynx
• Obstructive apnea: Restart NPCPAP if apnea recurs and wait for a week before weaning off CPAP. Watch for good weight gain or a weight > 1000 gms is reached.
• Don’t use CPAP for too long on a septic neonate, Resort to IMV early in the disease especially if the baby is preterm..
Length of NPCPAP: Should be optimized to about 5-7 cms from the nose to reduce the work of breathing
Anne grenough
Noninvasive respiratory support
CPAP can be delivered by a headbox, facemask, nasaopharyngeal or endotracheal tubes, single or dual nasal prongs, or a high-flow nasal cannula. Nowadays, the first two methods are rarely used. Studies have demonstrated that the method of CPAP delivery influences outcome. In one randomized trial, use of binasal prongs versus a nasopharyngeal prong was associated with a lower oxygen requirement and respiratory rate [13]. Meta-analysis of the results of two randomized trials evaluating CPAP following extubation demonstrated that short binasal prongs were more effective at preventing reintubation than a single or nasopharyngeal prong (RR 0.59 (0.41–0.85)) [13
In another study, however, the CPAP duration was shorter in very low birth weight infants when a nasopharyngeal prong was used rather than binasal prongs [14]. During ‘‘bubble’’ CPAP, the pressure in the device is generated by a continuous flow of gas with the distal end placed a set depth under water. The bubbles create pressure oscillations, which are transmitted back to the airway opening. Lung mechanics and applied flow influence the magnitude of the noise superimposed on the transmitted pressure wave form during bubble CPAP [15]. However, in a randomized crossover trial of 26 infants with a mean gestational age of 27 weeks, vigorous, high-amplitude bubbling compared with slow bubbling CPAP (each examined for 30 minutes) did not result in any significant differences with regard to respiratory rate, pulse oximetry, and transcutaneous carbon dioxide tensions [16].
It has been suggested that the chests of infants who receive bubble CPAP by way of an endotracheal tube vibrate in a similar manner and frequency to those who receive HFOV [17], and as a consequence it was hypothesized that bubble CPAP might reduce the work of breathing and augment gas exchange by facilitated diffusion. Lee and colleagues [17] were subsequently able to demonstrate that despite reduction in minute ventilation and respiratory rate on bubble CPAP compared with ventilator-derived CPAP in intubated infants, blood gas parameters were maintained. Variable flow CPAP is by way of nasal prongs or a modified nasal cannula, and the work of breathing is lower. The positive effects may result from gas entrainment by the high-velocity jet flows. Lung overdistension, however, may occur in infants who have mild disease if variable flow CPAP levels greater than 6 cmH2O are used.
Although nasal CPAP is considered by many as a gentler form of respiratory support [18], it does have adverse effects including nasal trauma. In some studies, this has been reported to be common; 20% of infants supported on dual prongs were affected in one series [19] and 32% in another [20]. It had been suggested that trauma may particularly be problematic with dual prongs, but randomized studies have demonstrated no significant differences in the incidence of trauma between binasal prongs and nasopharyngeal tube [14], or binasal prongs and facemask [20]. The only significant relationship to trauma in one series was CPAP duration [20].
Continuous negative distending pressure (CNEP) is an alternative way of providing distending pressure. The infant’s body is placed in a negative pressure box from which the head protrudes, and CNEP of -4 to -10 cmH2O is applied [21].
[13] De Paoli AG, Davis PG, Faber B, et al. Devices and pressure sources for administration of nasal continuous positive airway pressure (NCPAP) in preterm neonates. Cochrane Database Syst Rev 2002;4:CD002977.
[14] Buettiker V, Hug MI, Baenziger O, et al. Advantages and disadvantages of different nasal CPAP systems in newborns. Intensive Care Med 2004;30:926–30. [15] Pillow J, Travadi JN, Bubble CPAP. Is the noise important? An in vitro study. Pediatr Res 2005;57:826–30.
[16] Morley CJ, Lau R, De Paoli A, et al. Nasal continuous positive airway pressure: does bubbling improve gas exchange. Arch Dis Child Fetal Neonatal Ed 2005;90:343–4. [17] Lee KS, Dunn MS, Fenwick M, et al. A comparison of underwater bubble continuous positive airway pressure with ventilator-derived continuous positive airway pressure in premature neonates ready for extubation. Biol Neonate 1998;73(2):69–75 [18] Jacobsen T, Gronvall J, Petersen S, et al. ‘‘Minitouch’’ treatment of very low-birth-weight infants. Acta Paed 1993;82:934–8.
[19] Robertson NJ, McCarthy LS, Hamilton PA, et al. Nasal deformities resulting from flow driver continuous positive airway pressure. Arch Dis Child Fetal Neonatal Ed 1996; 75(3):F209–12.
[20] Yong SC, Chen SJ, Boo NY. Incidence of nasal trauma associated with nasal prong versus nasal mask during continuous positive airway pressure treatment in very low birthweight infants: a randomised control study. Arch Dis Child Fetal Neonatal Ed 2005;90:F480–3. [21] Samuels MP, Southall DP. Negative extrathoracic pressure in neonatal respiratory failure. Pediatrics 1989;98:1154–60.
Back