PERMISSIVE HYPERCAPNIA
Mechanical ventilation using high tidal volume (VT) and transpulmonary pressure can damage the lung, causing ventilator-induced lung injury. Several mechanisms have been offered to explain this damage ( Please refer to the chapter on ventilator induced lung injury ) . Increased mechanical stress may activate immune response in the lung, with the potential for intrapulmonary inflammatory mediators and bacteria to cross an impaired alveolar-capillary barrier. Therefore there is an emphasis on use of low-lung-stretch ventilatory strategies that reduce mechanical trauma and the associated inflammatory effects .
Permissive hypercapnia, a ventilatory strategy for acute respiratory failure in which the lungs are ventilated with a low inspiratory volume and pressure, has been accepted progressively in critical care for adult, pediatric, and neonatal patients requiring mechanical ventilation, and it is one of the central components of current protective ventilatory strategies. Permissive hypercapnia is used to minimize lung damage during mechanical ventilation . Hypercapnia is in fact not the goal of this approach, but rather a by-product of the attempt to limit airway pressures.
The limitations of this maneuver include the resulting hypoventilation, CO2 retention, and acidosis. Hypoxemia is caused by decreasing the alveolar oxygen tension and alveolar collapse during hypoventilation. The alveolar collapse can be offset in part, however, by increasing the end-expiratory volume.
PHYSIOLOGIC EFFECTS OFHYPERCAPNIA
Intracellular effects
Because of decreased CO2 elimination and consequent hypercapnia, respiratory acidosis occurs during hypoventilation. Acute hypercapnia decreases intracellular pH . The CO2 readily diffuses across cell membranes and, via the action of carbonic anhydrase, leads to the formation of carbonic acid and generation of hydrogen ions. Fortunately, intracellular buffering is rapid, reaching 90 percent completion within three hours after the onset of hypercapnia.
Effect on oxygenation
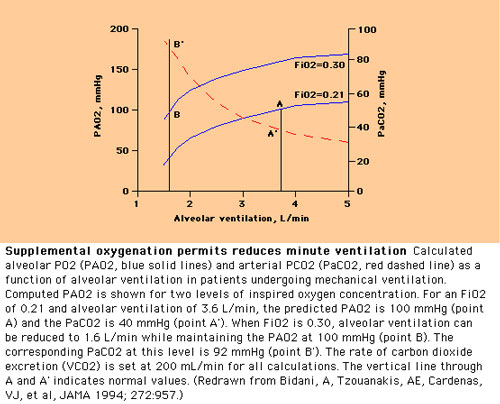
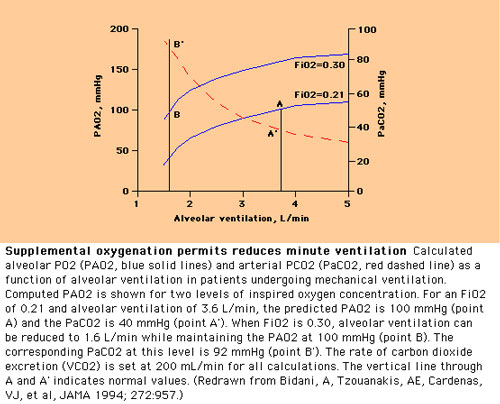
The reduction in minute ventilation with permissive hypercapnia ventilation ( PHV ) has the potential for lowering the arterial PO2. However, the use of supplemental oxygen during PHV allows for substantial reduction of minute ventilation without jeopardizing oxygenation . In addition, hypercapnic acidosis shifts the oxyhemoglobin dissociation curve to the right, thereby promoting oxygen release at the tissue level
Systemic effects
Laboratory studies have shown that acute hypercapnia, induced within 1 hour, is associated with significant increases in cardiac output, organ blood flow, and intracranial pressure.Systemic physiologic effects of hypercapnia in humans are respiratory (increased minute ventilation, subjective discomfort, air hunger, anxiety, fatigue), cardiovascular (increased cardiac output, tachycardia, systemic and pulmonary hypertension), neurologic (increased cerebral blood flow and cerebral edema), and metabolic (endogenous catecholamines and corticosteroids release, increased tissue O2 unloading and decreased effect of exogenous vasopressors). In extreme hypercapnia and in high-risk patients hypercapnia can cause myocardial depression and dysrhythmias, cerebral hemorrhage and herniation, stupor, and coma.
Acute hypercapnia increases sympathetic nervous system discharge. As a result, plasma levels of epinephrine and norepinephrine rise, leading to increased myocardial contractility and cardiac output.
Hypercapnia leads to cerebral vasodilation, increased intracranial pressure, and lowering of the seizure threshold.
The role of hypercapnia in protective lung ventilation per se, apart from the reduced lung stretch, remains unclear because of a lack of clinical data comparing the efficacy of protective lung ventilatory strategies in the presence and absence of hypercapnia. Experimental studies suggest that tissue oxygenation can be unchanged or improved during permissive hypercapnia with increased cardiac output, reduced differences in arterial and venous O2 content, and reduced blood lactate concentration. In dogs, permissive hypercapnia produced by inhaled CO2 produced gradual and significant increases in the hemoglobin concentration and arterial oxygen content, increasing oxygen-carrying capacity Animal studies of peripheral microcirculation showed that when PaCO2 increases up to 80mmHg, vessel diameter, blood-flow velocity, and blood-flow rate increase markedly, with slight increase in cardiac output; however, when PaCO2 exceeded 100 mm Hg, all these variables decreased. In addition, hypercapnic acidosis may reduce cellular oxygen demand.
In a study of the hemodynamic effects of hypercapnia in adult patients who have ARDS, the acute combined use of permissive hypercapnia, VT less than 6 mL/kg, distending pressures above PEEP of less than 20 cm H2O, and PEEP 2 cm H2O above the lower inflection point resulted in an immediate increase in heart rate, cardiac output, oxygen delivery, and mixed venous partial pressure of oxygen. The mean pulmonary arterial pressure increased markedly (by 8.8 mm Hg), but the pulmonary vascular resistance did not change. A multivariate analysis suggested that these acute hyperdynamic effects were related to respiratory acidosis, with no depressant effects ascribed to high PEEP levels, and transitory pulmonary hypertension and high cardiac output were attenuated significantly within 36 hours.
Hypercapnia and immune system
Hypercapnic acidosis attenuated acute experimental endotoxin-induced lung injury, improving the decrement in oxygenation and lung compliance and reducing alveolar neutrophil infiltration and histologic indices of lung injury. Hypercapnic acidosis may interfere with the coordination of the immune response. In one in vitro study, CO2 produced profound reversible inhibition of lipopolysaccharide- stimulated cytokine release by peritoneal macrophages, possibly explaining the lack of systemic inflammation after laparoscopic surgery with CO2. Macrophages incubated in CO2 produced significantly less tumor necrosis factor and interleukin (IL)-1 in response to lipopolysaccharide compared with those incubated in air or helium . These effects could be attributed to cellular acidification. According to some authors, neutrophils respond to hypercarbia by decreasing intracellular oxidant production and the release of IL-8 from lipopolysaccharide-stimulated cells. This hypothesis suggests that CO2 can modify neutrophil activity significantly by altering pH. Extracellular acidosis may intensify acute inflammatory responses by inducing neutrophil activation, delaying spontaneous apoptosis, and extending neutrophil functional lifespan. Hypercapnic acidosis may increase neutrophil CD18 expression and enhance neutrophil adhesion . There is a direct positive correlation between the intracellular pH value and the locomotor response of neutrophils to a chemotactic gradient.
Effect on neutrophil function
Spreading and several functions of neutrophils were observed to be inhibited at an acidic pH. This observation indicates that neutrophils release superoxide upon spreading, generating a burst of intracellular acid production, and the coordinated activation of intracellular pH regulatory mechanisms along with the oxidase is essential for sustained microbicidal activity. . Hypercapnic acidosis lessens inflammatory responses by blunting lung neutrophil recruitment, cytokine concentration, cell apoptosis, and the production of free radicals. It seems that acidosis protects the body's organ systems.
Antiinflammatory actions
Hypercapnic acidosis can have anti-inflammatory effects through a mechanism that inhibits activation of nuclear factor-kB, leading to down-regulation of intercellular adhesion molecule-1 and IL-8, which in turn inhibit neutrophil adherence to pulmonary endothelial cells.
Effect on free radical production
Hypercapnic acidosis seems to attenuate free radical production and may attenuate tissue injury following pulmonary ischemia and reperfusion. The production of superoxide radicals by chemotactic factor-stimulated human neutrophils in vitro was decreased at acidic pH. There are, however, concerns regarding the formation of nitration products from peroxynitrite, a potent free radical.
Beneficial effects of organ systems
In animal studies, hypercapnic acidosis reduced injury to the brain caused by hypoxia and ischemia. Other studies have looked at the function of acidosis in protecting myocardial tissue and reducing liver damage. The results are however disputing so far .
IMPLEMENTATION OF PERMISSIVEHYPERCAPNIA
Implementation of permissive hypercapnia requires ventilation with decreased VT and low alveolar pressure. The VT should be reduced gradually to 4 mL/kg or less to allow a progressive rise in the PaCO2, not to exceed 10 mm Hg/h, to a maximum of 80 to 100 mm Hg, to maintain arterial oxygen saturation (SaO2) greater than 90%. Higher levels of sedation may be required to manage patients with permissive hypercapnia
Contraindications to permissive hypercapnea
Because of its various physiologic effects, PHV is felt to be absolutely or relatively contraindicated in several settings: Due to the vasodilating effect of carbon dioxide, permissive hypercapnia is contraindicated in patients with cerebral trauma, cerebral hemorrhage, seizure disorder and lesions in the cerebrum . Inducing hypercapnia in these scenarios can worsen raised intracranial pressure .
Hypercapnea is relatively contraindicated in patients with hemodyanamic instability . Hypecapnea has been found to depress myocardial contractiliy . Because of its effect on sympathetic nervous system discharge, permissive hypercapnia has the theoretical potential for inducing cardiac arrhythmias. This concern has led authors to caution against its use in patients with heart failure, cardiac arrhythmias, or hypovolemia .
In the setting of hypovolemia, cardiovascular stability may be maintained by sympathetic discharge, and further increases in sympathetic discharge induced by PHV can augment the risk for cardiac arrhythmias.This is compounded by an impaired cardiac contractility with an acute increase in carbon dioxide level
Concerns have been raised about the use of permissive hypercapnia in patients with pulmonary hypertension and right heart failure, since hypercapnia increases pulmonary vascular pressures in animals .
Because of increased gastric hydrogen ion secretion in animal models of hypercapnia , the possibility of increasing the incidence or severity of gastric bleeding has been suggested as a potential consequence of PHV.
It has also been suggested that the concomitant use of beta blockers during PHV should probably be avoided , because blocking the effect of sympathetic discharge impairs compensation for the negative inotropic effects of hypercapnia and acidosis. There are concerns regarding the use of permissive hypercapnia in ventilated very-low-birth-weight infants during the first week of life, because impaired autoregulation during this period may be associated with increased vulnerability to brain injury. A retrospective cohort study of 574 very-low-birth-weight infants has shown that, in addition to traditional risk factors, the maximum PaCO2 during the first 3 days of life seems to be a dose-dependent predictor of severe intraventricular hemorrhage. According to Fabres and colleagues, both the extremes of arterial CO2 pressure and the magnitude of fluctuations in arterial CO2 pressure are associated with severe intraventricular hemorrhage in preterm infants, and it may be prudent to avoid extreme hypocapnia and hypercapnia during the period of risk for intraventricular hemorrhage.
Advantages
1) The strategy reduces the incidence of barotrauma as the tidal volume is limited in permissive hypercapnia ventilation
2) Achieves faster weaning
3) Improved survival
4) Decreased incidence of chronic lung disease
5) Improved long term Neurodevelopmental outcome
A study of physical outcome and school performance in a cohort of very-low-birthweight infants treated with early nasal continuous positive airway pressure and a minimal handling regimen with permissive hypercapnia found a relatively low incidence of handicaps and impairments, with near-average school performances that were not different from their siblings', indicating that these infants fare at least as well as survivors after conventional treatment.
Role of peak end expiratory pressures
Further development of this strategy emphasized the importance of alveolar recruitment by applying positive end-expiratory pressure (PEEP) and optimizing gas exchange. Although in most patients PEEP induces alveolar hyperinflation during mechanical ventilation with conventional VT, at low VT a significant alveolar collapse is present, and PEEP is able to expand these units, improving gas exchange and hemodynamics.
In patients who have Acute lung injury , a PEEP of at least 5 cm H2O is needed to prevent the decay of respiratory system compliance because of low VT ventilation.
 Managing hypercapneic acidosis
Managing hypercapneic acidosis
In critically ill patients, subjective discomfort caused by hypercapnic acidosis can be mitigated with the appropriate buffering and sedation. A slowly established hypercapnia, in which acidosis is buffered, would have minimal adverse effects. There are concerns, however, that the protective effects of hypercapnic acidosis in ALI result from the acidosis rather than CO2, and that buffering hypercapnic acidosis may worsen acute lung injury , causing pulmonary vasodilation.
Hypercapnia at normal pH also may enhance cell injury, as evidenced by the impairment of monolayer barrier function and increased induction of apoptosis via modifying nitric oxide-dependent pathways. In addition, CO2 can enhance nitration of surfactant protein A by activated alveolar macrophages and decrease its function.
Buffering with bicarbonate raises systemic CO2 levels and may worsen an intracellular acidosis.
Another option is the use of tromethamine acetate, which does not increase CO2 production. Tromethamine buffer may attenuate the reversible depression of myocardial contractility and hemodynamic alterations during rapid permissive hypercapnia and allow the benefit of decreased airway pressures to be realized while minimizing the adverse hemodynamic effects of hypercapnic acidosis. The role in neonates is not clear with this agent
Controversial issues
Permissive hypercapnea in sepsis and pneumonia
Hypercapnic acidosis has been found to inhibit the chemotactic and bactericidal activity of neutrophils and macrophages, render some antibiotics less effective, and potentially increase tissue destruction through neutrophil necrosis. In addition, a study by Stewart and colleagues, which included 42% patients who had pneumonia and 39% who had sepsis, suggested that permissive hypercapnia did not seem to reduce mortality and might increase morbidity.
Back